Cancer Treatment: A Systems Approach
Cancer cells, for decades regarded as a uniform mass of identical (“clonal”) cells, are not like the soldiers of a traditional army, trained to act and respond in unison. Cancer cells, even within a genetic clone, express enormous individuality akin to guerrilla fighters, each with unique strengths, weaknesses and distinct behaviors.

Cancer cells, for decades regarded as a uniform mass of identical (“clonal”) cells, are not like the soldiers of a traditional army, trained to act and respond in unison. Cancer cells, even within a genetic clone, express enormous individuality akin to guerrilla fighters, each with unique strengths, weaknesses and distinct behaviors. Therefore, they do not respond to an attack from a cancer drug in a uniform way. Rather, their responses are highly variable and often unpredictable. Only some die, while the survivors are changed – in different ways
There are three main challenges when it comes to cancer treatment:
- Cancer cells are too heterogeneous even for “broad-spectrum” drugs.
- There is a high failure rate in cancer-drug discovery
- Cancers can adapt to new targeted therapies and develop drug resistance.
When the first results of The Cancer Genome Project were reported, many scientists were shocked to learn that most patients, including those with the same type of cancer, did not share the same cancer-related mutations. This raised an obvious and disconcerting conclusion: If the patients’ tumors didn’t contain the same oncogenic mutations, then they likely didn’t share the same drug targets. The hopes that drove the initiation of the project, namely that we would identify the key oncogenic mutations shared across the various types of cancer, had been tempered with the realization of just how difficult it was going to be to develop “broad-spectrum” cancer drugs. It also highlighted the importance of stratification, not just at the level of the organs (brain cancer versus lung cancer, for example) but also at the level of patients with the same tumor type: Two patients with same nominal tumors may have different mutations. Now it adds a new level of heterogeneity: cells within the same tumor that became cancerous due to different oncogenic mutations, and cells with the same clone (harboring the same set of genes and mutations) are also different with respect to sensitivity to drugs.
This is part of a series on ISB’s systems biology approach to cancer research. Read the introduction or about
cancer detection and cancer stratification.
Even attempts to develop narrow-spectrum “targeted” cancer drugs, compounds that “target” a given tumor’s specific molecular Achilles Heel, often fail. Pharmaceutical companies spend an enormous amount of money and manpower in the research and development of cancer drugs. In 2013 alone, there were more than 200 new cancer drugs developed and tested for clinical trials. However, a recent report on the pharmaceutical industry observed that about 93 percent of cancer drugs fail during development. This is the highest failing rate among all drug discoveries*.
Part of the complexity is due to cancer cells utilizing key molecular pathways that are part of the exact same genetic programs that are needed for normal cell regeneration or wounding healing. It is extremely difficult to target these key pathways without affecting normal, healthy cells. The molecular pathways that control cell regeneration and growth are altered in cancer cells, allowing them to divide at a very high rate. Many chemotherapy drugs target these pathways in hopes of blocking the tumor’s ability to grow. Unfortunately, this also results in damage to the other rapidly dividing cells in the body. Intolerable side-effects to human patients are often the cause of cancer drugs ultimately failing near the late stages of clinical trials.
Cancers adapt to therapies and gain drug resistance
When an effective cancer drug with tolerable side-effects is successfully developed and used to treat a patient, the tumor unfortunately develops drug resistance within month and the treatment loses its effectiveness. How a tumor gains resistance to a cancer drug is a culmination of its unique characteristics described above, namely its high mutation rate, accelerated cell division, and as recognized recently, also cell-to-cell heterogeneity within genetically identical cells.
When an effective cancer drug with tolerable side-effects is successfully developed and used to treat a patient, it is almost always only a matter of time before the tumor develops drug resistance and the treatment loses its effectiveness. How a tumor gains resistance to a cancer drug is a culmination of its unique characteristics, namely its high mutation rate, accelerated cell division, and precisely, of cell-to-cell heterogeneity: each cancer cell is like a guerilla fighter, and has its unique way of evasion.
“If the patients’ tumors didn’t contain the same oncogenic mutations, then they likely didn’t share the same drug targets.”
Cellular heterogeneity means that in a tumor containing billions of cancer cells, at any point in time, you have a collection of cells with many small differences from their neighbors. Many of these differences are meaningless to the cancer cells harboring them. But a few of these mutations will change the cellular programs. When the drugs targeting these cellular programs arrive at the tumor and begin killing their neighboring cells, those with the right mutant are “invisible” to the drug: they have become resistant. Furthermore, some cancer cells will be induced to enter a drug-resistant state through epigenetic changes due to drug stress. Over time, these cells divide and re-establish the tumor with the drug-resistant “survivor” cancer cells.
What’s the solution? A widely proposed approach is to use a multi-pronged attack, using multiple targeted therapies directed at more than one molecular target in the cells – the rationale being that it is extremely unlikely that the cancer cells carry just the right set of mutations to make them invisible to not one but multiple drugs. This would be akin to winning the lottery several times in a row. However, this strategy also appears to fail.
The failure of current cancer treatments comes from the failure to understand the disease from its broader biological root. Since cancer is not caused by a single factor but from potentially hundreds of different genetic and epigenetic lesions that are not independent from each other, it is necessary to examine both the whole genome of the tumor and the systems-level mechanisms of cell state transition that serve as triggers. It’s then necessary to integrate all genetic and non-genetic factors into a network that explains the mechanisms of both cancer initiation and evolution. Treatments can be developed based on this network that drives cancer cells out of the rapidly dividing, rapidly adapting state back to a healthy or less-malignant state. But even then when relying solely on the “wiring diagrams” we still encounter failure. What also needs to be considered is that, despite having identical inner workings, each individual cell, for profound physics reasons, will be different from each other. It’s like how two identical lottery machines will produce different numbers. This difference can be amplified under therapy stress, which increases cell-cell heterogeneity and underlies the guerilla-like behavior of cancer.
How ISB Applies A Systems Approach to Treatment
‘Cancer State’ Theory
To reconcile all the paradoxes cancer research has encountered, Sui Huang’s lab at ISB has developed a novel theory of explaining the cause and progression of cancer called the “cancer attractor theory.” Rather than being a disease caused by genetic lesions accumulated over the lifespan of a person, the Huang lab proposes that cancer is actually a cell state, hard-wired into our genome, and that genetic mutations only enable this state to be accessed with higher likelihood. This “cancer state” is a remnant of a cellular program that was in our primordial ancestors which has undergone millions of years of evolution to survive and proliferate in harsh environments, such as low oxygen, high acidity, etc. Cell states similar to such unused states are accessed in embryonic development, wound healing and organ regeneration. And in a healthy person, the access of these stem-cell states is tightly controlled. Cancer ensues when mutations, which we call oncogenic, break this control mechanism. Then the ancient, highly resilient states, which have crude DNA repair mechanisms and hence are prone to accumulate mutations, become occupied. Their genetic programs, never used and adapted to the harmonious cell society of our normal tissues, becomes activated. If this theory is correct, then the goal of cancer treatment is not simply to kill more cancer cells, much as just increasing brute-force military power has never been a good strategy in guerilla warfare. Such attacks would cause the diversification of individual cells, already heterogeneous, into yet more ancient and stem cell-like state, not unlike dispersed guerilla fighters finding refuge in more rugged terrain. Instead, new drugs should be aimed at switching off the malignant state of cancer cells and driving them (back) to a more mature state with well-controlled proliferation, without stressing the inevitable surviving cancer cells.
Network Medicine
In a recent paper published by Sui Huang and Stuart Kauffman, they summarize a comprehensive new approach to treating cancer based on network medicine and understanding the heterogeneity of cancer cell populations. If cancer is a malignant state that is hard-wired into our genome and is perhaps the default state for cells placed under extreme stress, the current standards of treatment with highly stressful radiation or chemo-drugs will exacerbate the malignancy of the treated but not-killed cells. A better approach, they argue, would be to understand the gene regulatory networks that control the transition from a normal state to a malignant cancer state and develop gentle drugs to reverse this transition.
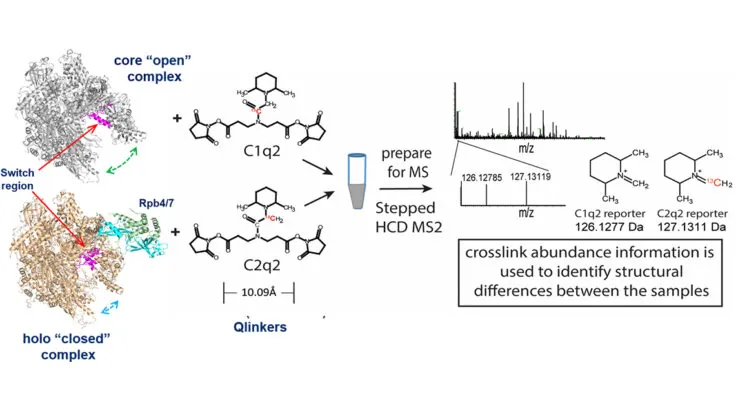
Cancer as a Chronic Disease
The latest breakthroughs in understanding stem cell biology and cell reprogramming have shown us that any cell, under extreme stress, can revert back to the more ancient, more stem-like state. At the ISB, researchers are seeking to shift cancer treatment from a strategy centered on eradicating all cancer cells, to one of coaxing the tumor cells to stop metastasis and enter a state of quiescence. Building on the approach of using network medicine to perturb cancer cells out of their malignant state, a member of the Sui Huang Lab, Joseph Zhou, is performing drug screens for molecules that could be effective at promoting this transition. From the more than 1,500 FDA-approved drugs analyzed, 16 were found to be non-cytotoxic (hence not imparting any stress that could make empower them to be fiercer guerilla fighters) and to promote the transition, of a breast cancer cell line into more mature and non-proliferative state. Anne Grosse-Wilde, also from the Huang lab, focuses on the aspect of cell heterogeneity and uses single cell analysis to discover new previously non-recognized cell states accessed by stressed cells that confer malignancy. The Jeff Ranish lab at ISB has developed a mass spectrometry-based technology that allows for the generation of high-resolution network maps of the proteins that control gene expression in cells in normal or malignant states. These maps not only show which proteins interact, but also how they interact. Having information about the protein interaction networks provides a roadmap that greatly facilitates the identification of proteins at critical interactions that can be targeted by modern drugs to cleanly nudge tumor cells into the non-malignant states without stressing them.